Topic: Seizure
Subject: Medicine
A 75-year-old male is brought to your office 1 month after a stroke that involved the left anterior cerebral artery, manifested by leg weakness, initial incontinence, and slowness in mentation. He experienced seizure activity on the second day after his stroke, but this was controlled by phenytoin (Dilantin). He has improved significantly and is now ambulatory. His family states that he now has episodic confusion, sleepiness, and clumsiness, which is preceded by paresthesias and dizziness, although no tonicclonic activity has been noted. He remains very drowsy for several hours after these episodes. He was wearing a cardiac monitor during one episode, but it showed nothing remarkable. His phenytoin level is therapeutic, and a CBC, metabolic profile, and magnesium level are all normal.
Which one of the following would be the most appropriate next step?
Discontinue the phenytoin
Add phenobarbital to the phenytoin
Begin bupropion (Wellbutrin)
Begin lamotrigine (Lamictal)
Correct Answer :
D. Begin lamotrigine (Lamictal)
Up to 50% of cases of epilepsy in the geriatric population result from cerebrovascular disease. Risk factors for post-stroke epilepsy include cortical involvement, hemorrhage, and large size. Approximately 35% of those who experience an acute stroke-related seizure develop post-stroke epilepsy, compared to only 9% of those who do not have acute seizure activity. The most common seizures in the elderly are complex partial seizures, but they do not have the typical presentation seen in younger people (aura, d�j� vu, olfactory hallucinations). Geriatric patients are more likely to have nonspecific preceding symptoms, such as vaguely localized paresthesias, dizziness, and muscle cramps. Those present may note episodic confusion, drowsiness, or clumsiness more than tonic-clonic movements. The postictal state is likely to be prolonged in the elderly. Misdiagnosis of these seizures is very common, with the diagnosis often delayed as much as 2 years from the time of the stroke. The most valuable diagnostic tool is a reliable history from those who witness the event.
Treating seizures in the elderly by using antiepileptic drugs (AEDs) is complicated by a number of factors. Pharmacokinetics are influenced by decreases in hepatic metabolism, renal elimination, plasma proteins, and protein binding. Many elderly patients are on a multiple-medication regimen that increases the risk of drug interactions, and many AEDs are enzyme inducing, which increases the risk of osteoporosis. The elderly also are more sensitive to side effects.
The choice of AEDs should be individualized, although many experts suggest early use of newer AEDs such as topiramate, gabapentin, lamotrigine, or levetiracetam because of fewer side effects and better pharmacokinetics. Monotherapy is preferred, if possible, and older drugs are less expensive, but limited by side effects.
In the case described here, the patient is having breakthrough seizures despite therapeutic levels of phenytoin. Switching to lamotrigine would be preferable and is less likely to cause side effects. When transitioning from one agent to another it would be best to gradually decrease the phenytoin rather than abruptly discontinuing it. The addition of phenobarbital would further increase drowsiness. Bupropion and modafinil may actually increase seizures.
Related Questions
Topic: Alzheimer's Disease
Subject: Medicine
Which one of the following is associated with an increased risk of developing Alzheimers disease?
A positive homozygous genotype for apolipoprotein E4
Elevated serum aluminum
Elevated serum alpha-tocopherol
Decreased serum Beta-carotene
Topic: Status Epilepticus
Subject: Medicine
A 58-year-old male with a history of seizure attacks suffered from a 30 min loss of consciousness with repetitive seizures with no recovery of consciousness between attacks. What is the disorder this patient is suffering from?
Tonic-clonic seizure
Absence seizure
Atonic seizure
Status epilepticus
Topic: Dementia
Subject: Medicine
Clinical features of multi-infarct dementia may include all of the following, except:
Parkinsonism
Deteriorating course
Evidence of cerebrovascular disease
Focal neurologic signs
Topic: Amnesia
Subject: Medicine
Which of the following medications may cause amnesia as a side effect?
Hydroxyzine
Fluoxetine
Triazolam
Clonidine
Topic: Organophosphate poisoning
Subject: Medicine
What is the mechanism of action in organophosphate poisoning?
Cholinesterase inhibition
Cholinesterase activation
Catecholamine inhibition
Catecholamine activation
Topic: Huntington disease
Subject: Medicine
A 42-year-old white male is brought to your department by his wife because of the progressive loss of his mental abilities, irritability, and some irregular involuntary movements of his hands. She says that she can remember when they were newlyweds, her husbands father had a similar condition at the age of 45 and he died few years later because there was not much doctors could do for him back then. She wants to know if their children may eventually develop a similar condition in the future. None in her family has ever had this type of condition. Which of the following would be the most appropriate answer?
Only their male children are at risk
If one child develops the disease, siblings are not at risk
All their children will inherit the disease
Each child has 50% risk of inheriting the disease
Topic: DM neuropathy
Subject: Medicine
In which of the following diseases would you see a gloves and stocking neuropathy?
Diabetes mellitus
Lupus
Multiple sclerosis
ALS
Topic: Tension headache.
Subject: Medicine
A woman presents with chief complaint of tightening, band-like headaches that usually occur upon rising in the morning. What is the most likely diagnosis?
Migraine headache
Premenstrual headache
Tension headache
Cluster headache
Topic: Huntington Chorea
Subject: Medicine
A patient previously diagnosed with Huntington chorea (HC) comes for a family planning consult with his wife. He states that his father had the disease and his mother was unaffected. They ask you what is the likelihood having a son with this condition?
Zero
25%
50%
75%
Topic: Temporal Arteritis
Subject: Medicine
A 75-year-old female presents with a 2-month history of bilateral headache, diffuse myalgias, and diplopia. On examination she has substantially diminished vision in her left eye, but no other neurologic findings. A moderately tender, cordlike structure is palpable just anterior to her ear and extending up to her lateral scalp. Blood tests show a markedly elevated erythrocyte sedimentation rate.
Which one of the following would be most appropriate at this point?
Clopidogrel (Plavix)
High-dose corticosteroids
NSAIDs
Dipyridamole/aspirin (Aggrenox)
Topic: Dementia
Subject: Medicine
An 85 year old white male is brought to you for the first time by his son. The father has recently seen a neurologist who performed a workup for dementia and diagnosed moderate Alzheimers disease. Which one of the following is true regarding the use of a cholinesterase inhibitor in this patient?
It is too late to initiate cholinesterase therapy
Agitation is often intensified by these agents
Memory is likely to improve significantly
Nursing-home placement may be delayed a year or longer
Topic: Horner's Syndrome
Subject: Medicine
A 66-year-old diabetic man presents with constriction of the pupil, drooping of the upper lid, and anhidrosis on the left. Which one of the following nerves is most likely involved?
Oculomotor
Sympathetic
Trochlear
Trigeminal
Topic: Adverse Drug Effect
Subject: Medicine
A 68-year-old man with a history of urolithiasis, suffered from a seizure attack which involved loss of consciousness with tonic and clonic muscular contractions. His tongue fell back into his throat and he choked. He is treated with valproic acid.
What are the most common side effects caused by this medication?
Weight gain
Rash
Nausea and headache
Tardive dyskinesia
Topic: Subarachnoid Hemorrhage
Subject: Medicine
A 36-year-old female presents with the sudden onset of severe headache, nausea, and photophobia. Her level of consciousness is progressively diminishing. Which one of the following would be the most appropriate next step?
Head CT without contrast
Head CT with contrast
Head MRI
Lumbar puncture
Topic: Subarachnoid Hemorrhage
Subject: Medicine
A 25-year-old male presents 5 hours after the onset of the worst headache of my life. His temperature is 37.0°C (98.6°F), blood pressure 140/90 mm Hg, respiratory rate 20/min, and pulse rate 90 beats/min. The patient is lethargic but oriented; there are no focal neurologic findings, but neck stiffness is present. Unenhanced CT of the head is negative. You elect to perform a lumbar puncture. At this time, which one of the following findings in bloody spinal fluid would indicate a diagnosis of subarachnoid hemorrhage?
Yellow-orange cerebrospinal fluid supernatant
A WBC:RBC ratio of 1/1000
A protein (g/L) to RBC (count/L) of 1/1000
A glucose level below 2.2 mmol/L
Topic: Seizure
Subject: Medicine
A 36-year-old male with a history of a seizure disorder is brought to the emergency department with generalized tonic-clonic activity. Emergency medical personnel report this has been ongoing for 20 minutes.
After initial resuscitative measures, the preferred medication in this situation is:
Phenytoin (Dilantin)
Fosphenytoin (Cerebyx)
Naloxone
Lorazepam (Ativan)
Topic: Essential Tremor
Subject: Medicine
Which one of the following is most likely to be of benefit in patients with essential tremor of the hand?
Isoniazid
Diazepam
Primidone
Clonidine
Topic: Alzheimer's Disease
Subject: Medicine
Which one of the following tests is most useful for the initial workup of suspected Alzheimers disease?
Carotid Doppler ultrasonography
An erythrocyte sedimentation rate
A cardiac stress test
A TSH level
Topic: Postherpetic Neuralgia
Subject: Medicine
A 78-year-old male comes to your office with a 3- day history of pain in the right side of his chest. The pain is described as burning and intense. Two days ago he noted a rash at that site. Examination reveals groups of vesicles on an erythematous base in a T-5 dermatome distribution on the right.
Which one of the following would be the most appropriate treatment to minimize the chance of post-herpetic neuralgia?
Famiciclovir (Famvir)
Prednisone
Capsaicin (Zostrix)
Carbamazepine (Tegretol)
Topic: Glasgow Coma Scale
Subject: Medicine
A 27 year old man is brought into the ER after a bicycling accident. A car door suddenly opened in front of him, of which he smashed into and was thrown 15 feet. On examination, he is drowsy and confused. He opens his eyes when his name is called. When he speaks, you understand his words but the sentences do not make sense. He moves all four limbs but does not respond to any commands. He is able to pull both hands away when pinched and squirms when his sternum is rubbed, making no effort to stop you.
What is his Glasgow Coma Scale score?
11
10
9
8
Topic: Horner's Syndrome
Subject: Medicine
A 70-year-old man presented with ptosis, myosis and anhydrosis on the left side. Which one of the following is the most likely cause of this condition?
Tumour induced exophthalmos
Fourth cranial nerve palsy
Apical pulmonary carcinoma
Enlarged thyroid gland
Topic: Horner's Syndrome
Subject: Medicine
A 70-year-old man presented with ptosis, myosis and anhydrosis on the left side. Which one of the following is the most likely cause of this condition?
Tumour induced exophthalmos
Fourth cranial nerve palsy
Apical pulmonary carcinoma
Enlarged thyroid gland
Topic: Mini Mental Status Exam (or MMSE)
Subject: Medicine
In healthy adults, performance on the Folstein Mini-Mental State Examination is affected by which one of the following?
Educational attainment
Socioeconomic status
Gender
Race
Topic: Heatstroke
Subject: Medicine
A 72-year-old male is brought to your office by a friend because of increasing confusion, irritability, and difficulty walking. This began shortly after the patients car broke down and he had to walk a mile to get to a phone and call the friend. The temperature outdoors has been near 39.5°C (100°F).
On examination you note a rectal temperature of 39.5°C (103.1°F). His pulse rate is 110 beats/min and his blood pressure is 100/60 mm Hg.
Which one of this patients findings indicates that he has heatstroke rather than heat exhaustion?
Confusion
Sweating
His temperature
His heart rate
Topic: Seizure
Subject: Medicine
Of the following, which is the most frequent cause of seizures in the elderly?
Alcohol withdrawal
Stroke
Head trauma
Hypoglycemia
Topic: Adverse Drug Effect
Subject: Medicine
Which one of the following is most associated with falls in older adults?
Diphenhydramine (Benadryl)
Atorvastatin (Lipitor)
Metformin (Glucophage)
Memantine (Namenda)
Topic: Temporal Lobe Lesion
Subject: Medicine
A 40 year old man presents with sporadically occurring behaviour automatisms and olfactory hallucinations. Which one of the following is the most likely diagnosis?
Schizophrenia
Schizophreniform psychosis
Hysterical personality disorder
Temporal lobe lesion
Topic: Mini Mental Status Exam (or MMSE)
Subject: Medicine
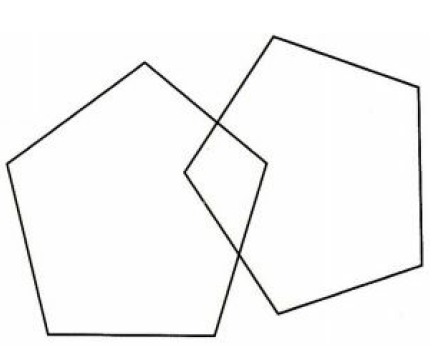
While performing the Mini-Mental State Exam the PCP asks her patient to copy the following design. What cognitive function is being assessed by this request?
Language
Orientation
Registration
Visual-motor integrity
Topic: Temporal Arteritis
Subject: Medicine
A female patient complains of a severe headache and jaw pain when she chews. She also complains of shoulder pain and bilateral wrist weakness. Initial lab tests show an ESR of 75 (normal is less than 30).
What is the most appropriate diagnosis?
Rheumatoid Arthritis
Temporal Arteritis
Polymyositis
Sarcoidosis
Topic: Fragile X Syndrome
Subject: Medicine
You are asked to see a mentally challenged 45-yearold male from a nearby group home who has groin pain. On examination you notice that he has large ears, a prominent jaw, and large symmetric testicles.
These findings are consistent with:
A variant form of Down syndrome
Aspergers syndrome
Klinefelters syndrome
Fragile X syndrome
